The Sub-Acute Phase: Crazy Dreams and Crazy Diet
The Social Worker at Primary Children’s Hospital told us that writing in a journal can be therapeutic. Even more, perhaps sharing our journey these past few weeks may help other families with children who suffer from this rare, devastating syndrome (F.I.R.E.S. = Febrile Infection-Related Epileptic Syndrome) or other chronic conditions.
Neuro Floor, Day #16 (Saturday, September 2nd)
65 days since onset. Seizure count = 2 Focal Seizures today.
2:00 PM: Drew really likes riding the bicycle for therapy. It is a three-wheel bike with two seat belts to help with trunk support and straps on both pedals to keep his feet in place. One therapist has to help from behind the bike to keep Drew’s head and trunk from sliding while the other therapist walks/runs next to the bicycle to help Drew steer. Again, his left arm is still quite weak, so he keeps veering to the left. The therapists were really trying to let him do more of the steering this time since it was a Saturday and there were fewer people on the pedestrian bridge between the hospital and the outpatient medical building across the street.
4:00 PM: “Never mind, Alex,” Drew said in frustration.
“What’s wrong?” Alex asked. He was helping Drew remember how to play Clash of Clans on his iPhone.
“My eyes can’t see the screen very well,” Drew said.
“Hold on,” Alex said. He crossed the room and pulled his iPad out of his backpack. After a few moments, he had the game pulled up on the bigger screen and tried again with Drew.
“I still can’t see it, Alex.” They tried for several minutes with the screen held only inches from Drew’s face, but he could not make out any of the details. “I can’t see it.”
As he went to return his iPad to his back backpack, Alex passed me in the chair watching them and he said, “Sad part is that Drew was the one that taught me how to play Clash of Clans when I got home from my mission last sumer. We would play together and kick butt all the time, even when I was in Kentucky we could team up together. Now he can’t play….”
“Hopefully his eyes will recover soon,” I said. Although at this point we are not certain if the visual problems are due to injury to the parts of his brain that process visual input, or if the problems stem from his eye muscles or focusing. At some point the doctors will have ophthalmology return to screen his vision and make recommendations.
7:20 PM: “Dad, the game starts in 10 minutes.”
Drew was not happy with me and his mother because we insisted he get out of bed and go for a quick wheelchair ride to the patio. He hadn’t been out of bed since the bike ride in therapy and we knew he wouldn’t get up once the game started.
“We’ll be back in time for kick-off,” I said to Drew as we rolled down the hall to the elevators.
“Is that Drew?” Two nurses from the ICU approached us from the other end of the hallway as they had just finished shift change.
“Hello,” Drew said as he waved his right hand. “My name is Drew. Who are you?”
“I took care of you in the ICU a few weeks ago while you were sleeping,” the nurse explained to him. I recognized both of them and smiled, but Drew had no idea who they were (again, not sure if it was due to his eyesight or his memory, but probably a combination of both).
After we talked a few minutes, the nurses had to leave. “We’ll see you later, Drew.”
“OK,” he replied and waved his right hand, “Bye.”
As the nurses continued walking toward the stair leading to the lobby, the one nurse turned to the other and said, “Well that just made my day!”
8:45: One of the rehab doctors this morning challenged Drew to an arm wrestle to test his strength, but he struggled to even hold his grip, especially on the left hand. So the doctor instead challenged him to a thumb war, and Drew actually won both the right hand and the left hand. The doctor was amazed and assured me he had been trying to win, but Drew beat him. As a result, Drew challenged the two male nurses tonight to thumb wars as they gave him his medicines. He still gets the 4 Anakinra shots along with 6 seizure medications, vitamins, and an antibiotic all crushed up and administered through his feeding tube, so it takes quite a while for all of the medicines to be given. However, Drew actually beat both of the nurses as well. The one nurse laughed as Drew pinned him and said, “he has such long thumbs, and they are strong.”
Drew actually became more interested in the thumb wars with the nurses instead of the BYU football game against LSU on TV because he really couldn’t see the screen very well. We had to keep letting him know the score and clock and other info about the game because he couldn’t read them on the screen. However, within minutes of getting his last medication, he fell asleep just before halftime. We turned the TV off so he could sleep and his older sister, Erin, volunteered to stay with him so the rest of the family left for home as they settled down for the night.
Neuro Floor, Day #17 (Sunday, September 3rd)
66 days since onset. Seizure count = 1 Focal Seizure today.
8:30 AM Erin reported that Drew awoke at 1:30 AM, 3:30 AM, and 6:30 AM for various reasons, so we talked to the doctors and nurses about scheduling some rest breaks during the daytime to help him stay awake later into the evening. We also agreed to let them give him some Melatonin to help him get back into a better sleep pattern at night. Once he was up for good at 6:30 AM, his sister turned on The Amazing Spider Man Part 2 for him to watch. She played the movie on her laptop computer and set it up on two pillows on his lap where he can see the screen better, even if he can’t make out all of the details.
11:00 AM: Drew went to church at the hospital with his mother and older sister for the first time this morning. He couldn’t take the bread, but he took the water as the Sacrament was passed.
When I returned to the hospital later in the afternoon, I asked, “So how did you like church, Drew?”
He answered, “I couldn’t really understand what the people were saying and a lot of them just cried.” As today was the first Sunday of the month, church consisted of a Fast and Testimony Meeting, and his mother explained that many of the people who shared their testimonies either talked too fast or too softly for Drew to be able to understand what they were saying.
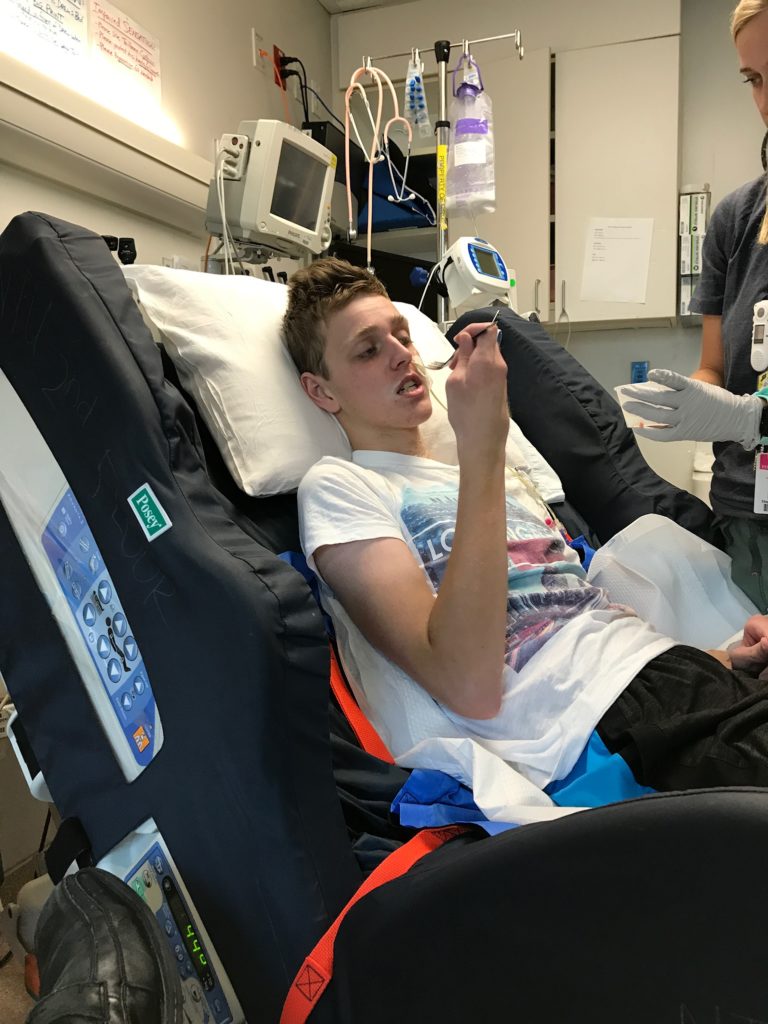
6:30 PM: When I returned to the hospital after my church meetings were finished, his mother reported that Drew sat up in a chair next to his bed for a couple of hours in the afternoon and used the dry-erase board to work on some math, writing, and memory cues. He also watched a little bit of “My Fair Lady” with his mother and sister. I had to laugh because he challenged his brother and uncle and some of his visitors to thumb wars.
Neuro Floor, Day #18 (Monday, September 4th)
67 days since onset. Seizure count = 1 Focal Seizure lasting about 70 minutes
9:15 AM: Drew started having a seizure at 8:58 this morning. It was a Focal Seizure where his eyes rolled up and deviated to the side, but it was quite sudden. He had been fully awake and talking to me and the nurses. We were going to get him up into a wheelchair for the morning because we found out with the Labor Day holiday today, therapy would not be coming to work with Drew until after lunchtime. So the nurse had just rolled Drew’s wheelchair into his room and I knelt down to remove the leg rests. When we turned back around to help Drew, he was having the seizure.
“Are you sure it’s a seizure?” The nurse asked me.
“Yes,” I said. “This is what the last several seizures have looked like, although sometimes he has more mouth twitching.”
A few moments passed as we waited for the seizure to stop, and at one point, his right eye stayed rolled up and deviated to the right while his left eye rolled downward and deviated in the opposite direction and looked really freaky. At that point, seven minutes had passed without the seizure breaking, so the nurse notified the attending doctors and she went to go get his “rescue medicine,” which is a dose of Ativan. We had requested more specific guidelines from Neurology as to when he could get a “rescue” medicine to help break him out of a prolonged seizure, or cluster of seizures, and they had specified for him to get the medicine if he has a General Tonic-Clonic (Grand Mal) that lasts more than 5 minutes, or a Focal Seizure that lasts more than 10 minutes. By the time the nurse returned with the medication, 12 minutes had passed without the seizure stopping, so she gave him the medicine through his IV.
9:35 AM: The doctors just gave Drew a third dose of Ativan to try and stop this seizure. The first two doses seemed to work for about 30 seconds each time, but then he went right back into the seizure.
“If we cannot get the seizure to stop, we may have to transfer him back to the ICU,” the doctors told us.
“No,” Dawn said as she leaned closer to Drew and squeezed his hand. “Come on, Drew. Wake up!” Tears were streaming down her cheeks.
9:55 AM: Despite the third dose of Ativan, his seizure did not stop and the group of hospitalist doctors in the hallway talked with the Neurology doctors. They agreed to try one more medicine — a dose of Fosphenytoin — which is more powerful, but also has more side effects.
“If the Fosphenytoin doesn’t work, or if his breathing starts to becme suppressed with all of the medicines on board, we will have to move Drew to the ICU,” the doctors told us while the nurses worked frantically to hook up the IV pump that would administer the medicine. “We also need to hook him back up to an EEG for the next several hours to help us watch for any more seizure activity.”
Dawn collapsed in a chair and started to sob. I tried to comfort her and rubbed her shoulders as we watched the commotion going on around Drew’s bed. “Don’t cry,” I said to her. “It will be all right. Drew will pull out of this.”
“Today wasn’t supposed to be like this,” she said. Then angrily, she looked up at me and added, “And there’s no way I want to go back to that hellish nightmare.”
I am fearful that if Drew does have return to the ICU, Dawn may have some PTSD and be pretty traumatized by the setback.
11:30 AM: It took about 15 minutes for the full dose of Fosphenytoin to run into Drew’s IV and it appears to have finally stopped the seizure, so we were able to avoid transferring back to the ICU for the moment. However, all of the medicines have made Drew extremely sleepy and dropped his blood pressure down to 85/42. The nurses are pushing fluids through his IV to help raise his blood pressure back up. Meanwhile, the doctors are running a bunch of tests to try and figure this out, and they are getting ready to hook him back up to an EEG for a little while. They plan to watch him closely for the next several hours to make sure his seizure has stopped and his breathing stays good.
9:00 PM: Drew is doing much better tonight. The Ativan is finally wearing off and he is back to talking and laughing and hugging everyone. He helped us sing “Happy Birthday” for my birthday tonight. He had one 30-second seizure this afternoon, but otherwise his seizures have been fine since the big one this morning. They really coudn’t identify any reason for the prolonged seizure, and the Neurology doctors are not even sure they want to call it a seizure, but rather they are referred to it as an “event.” His labs came back good. His Phenobarbital level was in range. Nothing else really changes, so they aren’t sure what cause the “event.” Hopefully we are back on schedule tomorrow with rehab and maybe even removing the tracheostomy, but we’ll see what the doctors decide.
Neuro Floor, Day #19 (Tuesday, September 5th)
68 days since onset. Seizure count = No seizures today.
3:00 AM: “Dad,” Drew yelled. “Dad!”
“What’s the matter Drew?” I answered from the fold-out couch in the corner of the room.
“Get her away from me,” Drew yelled as he tried to hit the nurses’ aide sitting beside his bed. At night, he continues to require a 1-on-1 nurses’ aide to keep him from pulling out his tubes.
“Drew, be nice,” I said.
“Get away!” Drew continued to yell and swing. “Dad, get me out of here!”
It took us several minutes to calm him down. Every morning he has been waking up between 2:00 and 4:00 and started pulling at his IV and feeding tube and breathing tube. He often forgets he is still in the hospital and starts swinging at the nurses and aides, but I have been able to talk to him and calm him down. Luckily, he fell back asleep this morning after about 25 minutes of yelling.
4:00 PM: The EEG came off about 2 hours ago and his hair is all gummed up with the glue from the 19 different leads that had been attached to his scalp. The nurses and his mother plan to give him a bath this evening and work on getting all the EEG glue washed out of his hair.
9:00 PM: No seizures today. Drew was able to participate in all of his physical, occupational, and speech therapy sessions, but he did fall asleep during both speech therapy treatments. His speech has been a little slurred and his responses a little delayed today, so they think he may still have a little bit of the rescue medicines in his system, but overall a much better day than yesterday.
The doctors told us today that they plan to try and increase Drew’s therapy treatments this week to see if he can tolerate 3 hours per day. So starting tomorrow he will have separate PT, OT, and Speech treatments in the morning and again in the afternoon, as well as Music Therapy from 3:30 to 4:30. His Rest Breaks will remain the same for now. Even though his tracheostomy was capped all day today with no problems, the doctors are talking that they may postpone taking the tracheostomy out for another day or two just in case he has more seizures like yesterday, but we will talk to them tomorrow and try to move it up since he had no seizures today. It just goes to show that so long as the seizures stay away, he will continue to do great.
Neuro Floor, Day #20 (Wednesday, September 6th)
69 days since onset. Seizure count = No seizures today.
2:45 AM: I awoke to the sound of a ‘crash.’
“Where do you think you are going?” The nurse’s aide said as she ran into our dimly-lit room. I then realized that Drew had swung his legs over the bed rail and was trying to climb out of bed.
“Whoa,” I said as I jumped up off the fold-out couch and ran to the side of Drew’s bed. I arrived before the nurse’s aide and grabbed his legs to keep him from getting out of bed. “Drew, stop.”
“Pull me up, Dad,” Drew said, speech slurred, eyes half-open. “Help me out of here.”
“No, Drew,” I said. “You need to stay in bed.”
“Get me out of here, Dad.”
“You’re OK,” the nurse’s aide said. “Let’s go back to sleep.”
“Help me, Dad.”
“I’m right here, Drew.” I pulled up a chair and sat next to his bed, holding his hand. It took about 30 minutes for him to fall back asleep again.
4:00 AM: Just as I was falling back asleep, Drew tried crawling out of bed again. We stopped him and repeated the same routine to keep him in bed and help him fall back asleep.
7:00 AM: “Can you help me brush my teeth, Dad?”
“Sure, Drew.” I handed him his tooth brush with a pearl of Ketogenic-friendly toothpaste and assisted him with brushing and rinsing his teeth.
After he finished putting on chap stick, as we were waiting for nursing to bring his medications and occupational therapy to start at 8:30, we sat talking.
“Did you have a bad dream last night?” I asked Drew.
“Yeah,” he said. “I had a dream that I was in a tomb full of mummies and I was trying to get out of it.” He continued to describe the dream to me, and then it made perfect sense why he was confused and trying to get out of bed a few hours earlier.
4:00 PM: We didn’t even have to discuss the tracheostomy schedule with the doctors. The Respiratory Therapy Director came into Drew’s room this afternoon and announced that it was time to remove the cannula. She explained that based upon his capping trial tolerance, there was no need to postpone taking out his tracheostomy, so she carefully removed it and covered the fistula with a small bandage. She explained that the hole will heal over time on its own and to just keep it clean and covered so nothing enters into his throat and lungs until it heals.
When I arrived from work, Drew’s eyes lit up and he said, “Hey, Dad, I have a hole in my throat.” The bandage over the hole was flapping around the edges as Drew’s voice was nearly blasting the cover off. His words were breathy because of the hole in his throat, but I could make out what he was saying.
Lastly today, with the tracheostomy removed, speech therapy scheduled him for a swallow study on Friday and she brought in some real food to start practicing eating. Her options were limited thanks to his Ketogenic diet, but she brought in some fresh avocado and Drew loved it.
Neuro Floor, Day #21 (Thursday, September 7th)
70 days since onset. Seizure count = No seizures today.
7:30 AM: Drew had a really bad night again last night. He woke up screaming for me three different times. The nurse’s aide was no longer able to help after 6:00 AM this morning, so I was sitting next to Drew’s bed watching him when he started talking in his sleep.
“It’s still looking at me, Dad.” His eyes were half-open and it seemed like he was looking through me at something on the wall.
He recoiled and tried to move away from me in the bed, “Help me, Dad.”
“I’m right here, Drew.” I held his hand as he slowly fell back asleep.
8:25 AM: The nurse just finished giving Drew his medications, and we had a few minutes until the OT would arrive to start his treatment, so we were talking again and Drew was telling me about the crazy dream he was having this morning.
“You were there with me, Dad. We were helping Santa Claus in his sleigh, and as we were flying along with the Christmas Spirit, I looked down and saw a bunch of baby moose. We stopped to look at them, and then I saw a big moose that was trying to kill me with his antlers.”
On the one hand, Drew is finally getting more sleep. But on the other hand, he is having really vivid, crazy dreams. Hopefully these will continue to resolve as his brain heals.
4:45 PM: So Drew will be officially transferring to the Rehab Team tomorrow afternoon. He will be getting evaluated and tested by the Rehab Team over the Weekend and then on Tuesday, they will have a better estimate of how much longer he will be in the hospital. Right now they are estimating 3 to 5 weeks in Rehab, and then outpatient therapy once we get home. Because of his brain injury, he will need to be supervised 24/7 for several weeks after he returns home. The plan is to keep him on all 7 of his medicines and the Ketogenic diet for at least 2 months before making any changes. As the Rheumatology doctor explained, they feel like his inflammatory system has finally calmed down and they want to keep it calm while he rehabilitates. Down the road, they can revisit his diet and medicines to see if they can be decreased without allowing the seizures to return, but for now, status quo — and really, other than the one bad seizure last Monday, his seizures have been doing really well.
Rehab Team, Day #1 (Friday, September 8th)
71 days since onset. Seizure count = No seizures so far today.
10:00 AM Drew had a pretty good morning so far. He slept a little better last night because I kept the light above the sink on all night. He still woke up at 2:00 AM thinking he had to go to school, but with the light on, he was able to remember more quickly that he was in the hospital and It took less time to calm him down. He also got up with OT this morning and got himself dressed (with a little help) and then PT worked his legs really hard in the gym. He came back almost asleep in the wheelchair, so we laid him back down and he is taking a nap. Swallow study is supposed to be at 11:00 and then this afternoon he will be officially transferred to Rehab.
Noon: Drew passed the Swallow Study with flying colors. The Speech Therapist gave him some water and pudding mixed with barium, and then she and the Radiologist watched on X-ray as Drew swallowed. He needed a little water to wash some residual pudding down, but otherwise he swallowed without coaching or problems.
3:30 PM: Drew had his first meal with Speech Therapy this afternoon. Once he was cleared by the Swallow Study, he was allowed to practice a full, Ketogenic tray of food. The Speech Therapist brought a tray of chicken, bacon, avocado, salsa, butter, and heavy cream. Drew freaked out with the smell of the bacon and said it was going to make him throw up, so we had to get rid of the bacon initially. He ended up eating the chicken, salsa, and avocado with the butter and heavy cream mixed in to raise the fat ratio. He also drank some water. He will start getting some trays now at meal times to see if he can start eating, but because of his crazy, Ketogenic diet, it will be heavy on fats with very few proteins and practically no carbohydrates. The Speech Therapist laughed and said Drew is the first Ketogenic patient she has worked with here who was actually eating the Ketogenic food and not just getting all of his nutrition through his feeding tube. We’re all going to be learning this strange diet together since Drew will be on it for at least two months.
4:30 PM: The Rehab Doctor stopped in to talk to us briefly. She has written the orders and now Drew has been officially admitted onto the Rehab Team.
WELCOME TO REHAB!!!
© Copyright 2017 Jeff, All rights Reserved. Written For: Jeffrey Olsen






Prayers continuing for you all. Maybe it is the combination of the medicine making his dreams so crazy. We hope he continues to improve.
Give Dawn a big ((HUG)) for me! We’ll keep praying!! 🙂
You don’t know me but a friend of mine who teaches at Copper Hills High has been sharing links to your blog, which I follow frequently. I have been praying for Drew and all of you for continued peace and strength, as well as healing for Drew. Thank you for sharing this journey. It has helped me start to believe in miracles again.
Prayers continue for Drew,and all of the rest of your family.
I just wanted to mention that I sometimes need to take melatonin to sleep. Almost every time I do, it causes very vivid and strange dreams. I don’t know if Drew is using it to help him sleep, but maybe a lower dosage might be better for his scary dreams.
I’ve been following Drew’s story since the beginning and my heart and soul is invested in him, your family and his success. Sending love and prayers your way!
What a great update! Glad Drew has made such significant progress. Praying for his rehab and recovery every day.
What an amazing young man and persevering family. You all inspire so much. Thank you for sharing your story! God bless!
Is Drew still getting Melatonin? My family has experienced a plethora of crazy realistic dreams while on different doses of Melatonin. I’m so glad to hear of how well Drew is doing! ❤
I’m another who has been following Drew’s story for a long time now, and I’m so happy to hear of all his progress and continue to wish and pray for the best for him and your family!! I also wanted to suggest that probiotics may be very helpful/important for him since he has been on antibiotics for so long (and a healthy gut is a very important part to healing). I hope he continues to do better and that things keep looking up for him!!!
I have been following along for many weeks now! Great to see such progress. I am one of the many who cannot use Melatonin because of the nightmares it causes, and I was wondering if it was affecting Drew the same way. Huggs to you all.
Not sure yet, but he was having nightmares and vivid dreams prior to starting the Melatonin. Once his sleep cycle returns to normal they plan to discontinue it.
I found your blog from the hashtag DrewStrong on social media. My husband and I serve with the branch at the hospital. We met him today while giving him the Sacrament. We are praying for him and your whole family!